Recent Posts
HPHS Mission
Disseminate and increase knowledge about the normal and diseased liver and biliary tree, with special emphasis on Pathology – and encourage the further development of hepatopathology as a subspecialty.
-
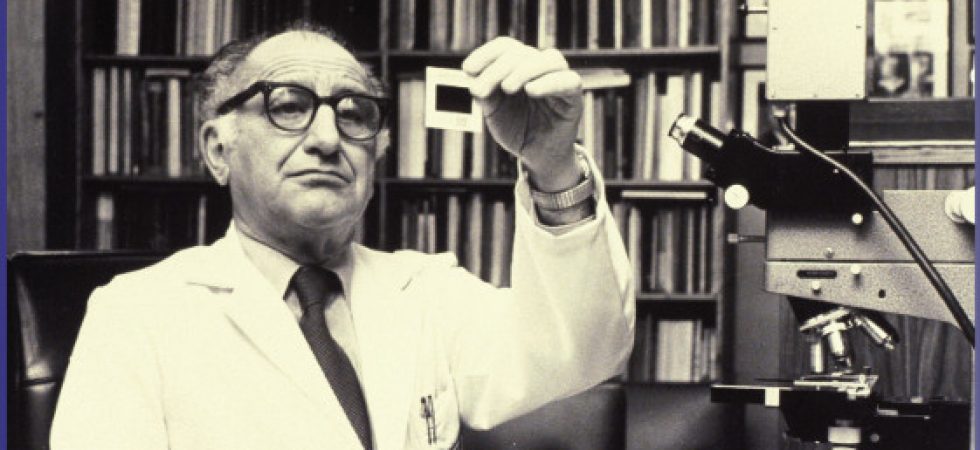
Lifetime Achievement Award
Congratulations to the 2022 recipients!
-
Trainee Best Abstract Award
Congratulations to our 2023 winners!Click here for details Applications for the Best Abstract Award are open. More info and application details will be posted here. The HPHS Trainee Award is…
-
Dues Payments & Donations
The Hans Popper Hepatopathology Society is a tax-exempt (501(c)(3)); therefore your membership dues and donations are tax-deductible. The Hans Popper Hepatopathology Society has an EIN (Federal Tax Identification Number for…